Gabon, The Forgotten Promise of 15%: When Underfunding in Health Costs Lives


15% on the front, health in apnea: the Gabonese budget on life support
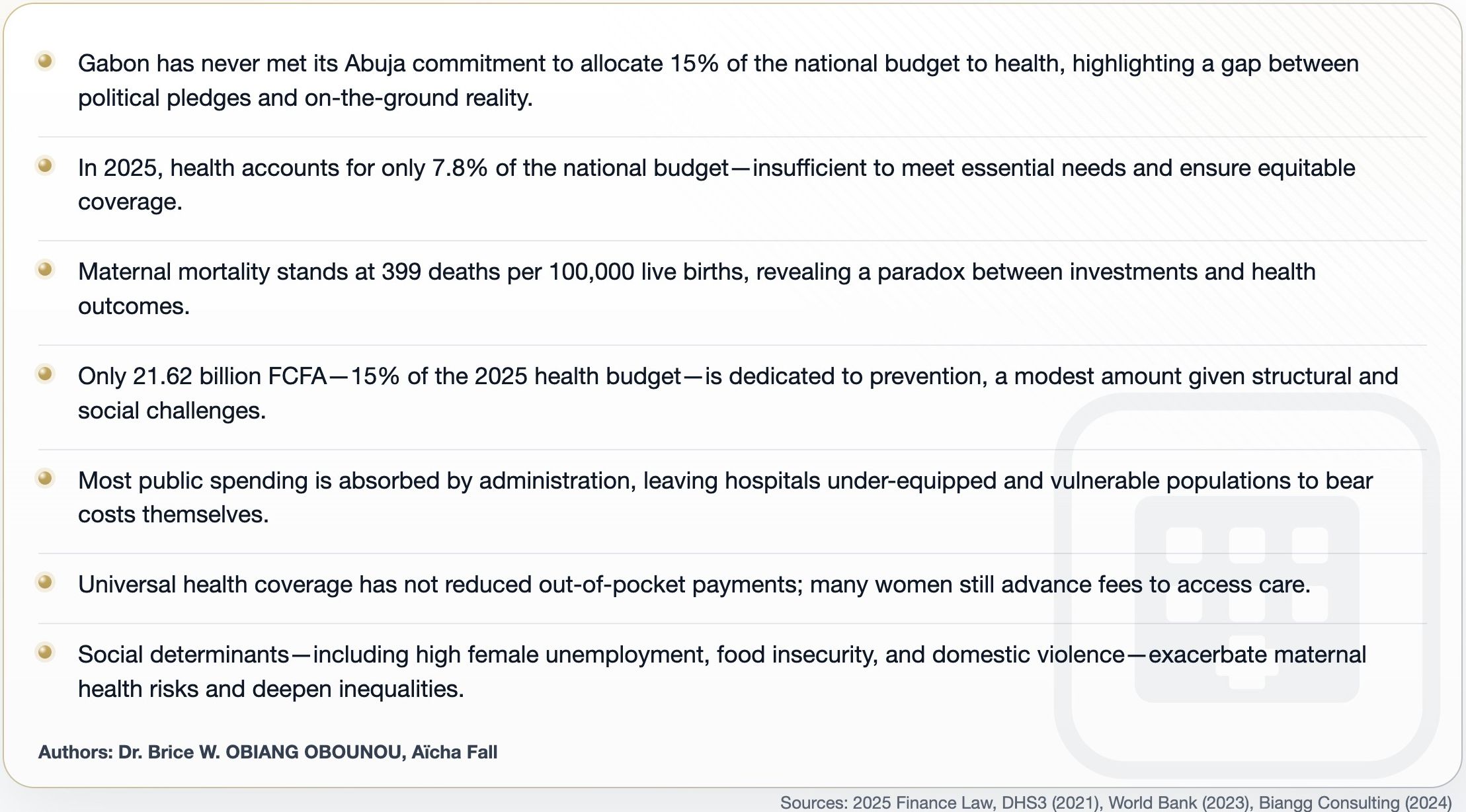
Key insights
Key figures
“To date, the overall resources allocated to health in Gabon have not contributed to improving health outcomes” - Brice Wilfried Obiang Obounou, Financing the health system and maternal mortality in Gabon.
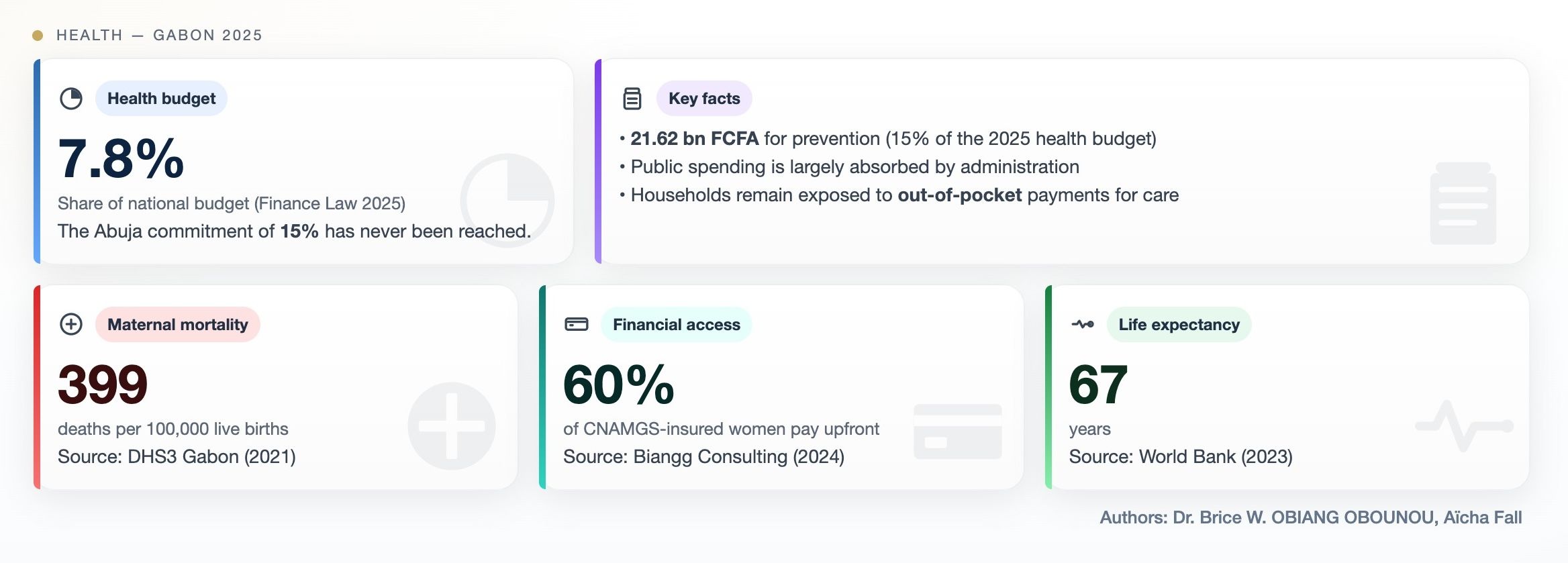
These words strike with their sobriety and lucidity. They summarize twenty years of thwarted efforts, growing budgets, and always fragile indicators. Gabon, a pioneer in Central Africa for universal health coverage, has never fulfilled its Abuja commitment. 15% of the national budget was to be dedicated to health, but the country currently caps at 7.8% according to the finance law.
Behind this figure lies a distressing contradiction. Life expectancy is increasing, infrastructure is modernizing, and yet mothers continue to die in rural maternity wards as well as in urban hospitals. The work of Brice Wilfried Obiang Obounou sheds light on this fracture between ambition and reality, between symbolic and tangible, revealing the human cost of ineffective funding.
The forgotten oath of the African continent

In Africa, leaders gathered in Abuja in 2001 to commit to dedicating 15% of their national budgets to health. This pact was to transform the face of public health and provide every citizen with effective access to care. A few low-income countries like Rwanda, Malawi, or Gambia have exceeded this commitment, showing that wealth was not a condition for investing in life.
But in many resource-rich countries, ambitions have collided with divergent priorities and the complexity of administrations. Sector spending often remains insufficient and oriented towards operations rather than populations. The figures reveal a deep contradiction. The richer a country is in natural resources, the less it seems to invest in the lives of its populations.
Central Africa between ambitions and realities
Central Africa wanted to believe in universal health coverage and its promises. Institutions multiplied, plans and programs accumulated, but implementation faces structural and financial limits. Administrative expenses absorb most of the budgets, and prevention as well as primary care remain insufficient. Gabon was long perceived as a regional model thanks to the creation of CNAMGS (National Health Insurance and Social Guarantee Fund) in 2008. This system was to provide equitable access to care. In practice, it faces payment delays, exclusion of the private sector, and bureaucratic complexity. Vulnerable populations continue to pay for their care, sometimes at the cost of debts or sacrifices.
Gabon and the paradox of unfinished progress
The 2025 health budget of Gabon represents 7.8% of the national budget, a figure that reflects a gap between ambitions and means. The majority of funds are absorbed by administration and fixed costs, leaving hospitals and maternity wards under-equipped and vulnerable populations reliant on their own budget.
Despite visible progress in life expectancy and infant mortality, maternal mortality reaches 399 deaths per 100,000 live births, signaling a crisis that is not resolved by increasing the budget or modernizing infrastructure. Each death tells a story. A woman giving birth alone in a dispensary, another who has to buy her medications, a third who travels through several villages to reach a hospital. These lost lives reveal the gap between spending and real impact.
When health becomes a luxury

Universal health coverage has not eliminated out-of-pocket payments. In private clinics, 60% of women insured by CNAMGS still pay upfront. The poorest, often in rural areas, face endless queues and drug shortages. This social and geographical divide creates a two-tier system. The wealthy access care quickly and efficiently, while others forgo it or suffer delays with often fatal consequences.
High female unemployment, food insecurity, and domestic violence exacerbate this situation. Women from low-income households hesitate to use health services for fear of costs or delays. These social determinants directly increase maternal mortality and fuel inequalities.
Prevention, a still fragile link
Prevention accounts for only 21.62 billion FCFA, or 15% of the health budget in 2025. This funding remains insufficient given the structural and social needs weighing on the population. Vaccinations, prenatal care, screenings, and nutritional programs are essential to reduce maternal and infant mortality.
Every franc invested in prevention could save several lives and reduce costs related to avoidable complications. The priority given to curative care at the expense of prevention weakens the system and deepens disparities between urban and rural populations.
Relearning to invest in life
It is no longer just about how much the country spends, but how it spends. The budget must be redirected towards prevention, equitable access to care, and reducing social inequalities. Health must become a pillar of the social contract again, not a variable of budgetary adjustment.
The 15% of Abuja was not a statistic but a human commitment. Failing to reach it means accepting that health remains a matter of privilege and that the lives of thousands of mothers continue to hang in the balance due to slow budgets.
Gabon can still transform its trajectory, but this requires a clear vision, genuine commitment, and effective resource allocation so that numbers finally translate into saved lives and restored dignity.
About the authors: Brice is the founder of Biangg Consulting, specializing in patient advocacy and health equity. Aicha Fall is an economic journalist.

